Scientists find hidden brain source that fuels dementia
- Date:
- November 6, 2025
- Source:
- Weill Cornell Medicine
- Summary:
- Weill Cornell researchers uncovered how free radicals from astrocyte mitochondria can fuel dementia. Using new compounds that target these radicals at their source, they slowed brain inflammation and neuronal damage in mice. The findings reveal a potential breakthrough for treating diseases like Alzheimer’s and frontotemporal dementia by focusing on the precise mechanisms driving degeneration.
- Share:
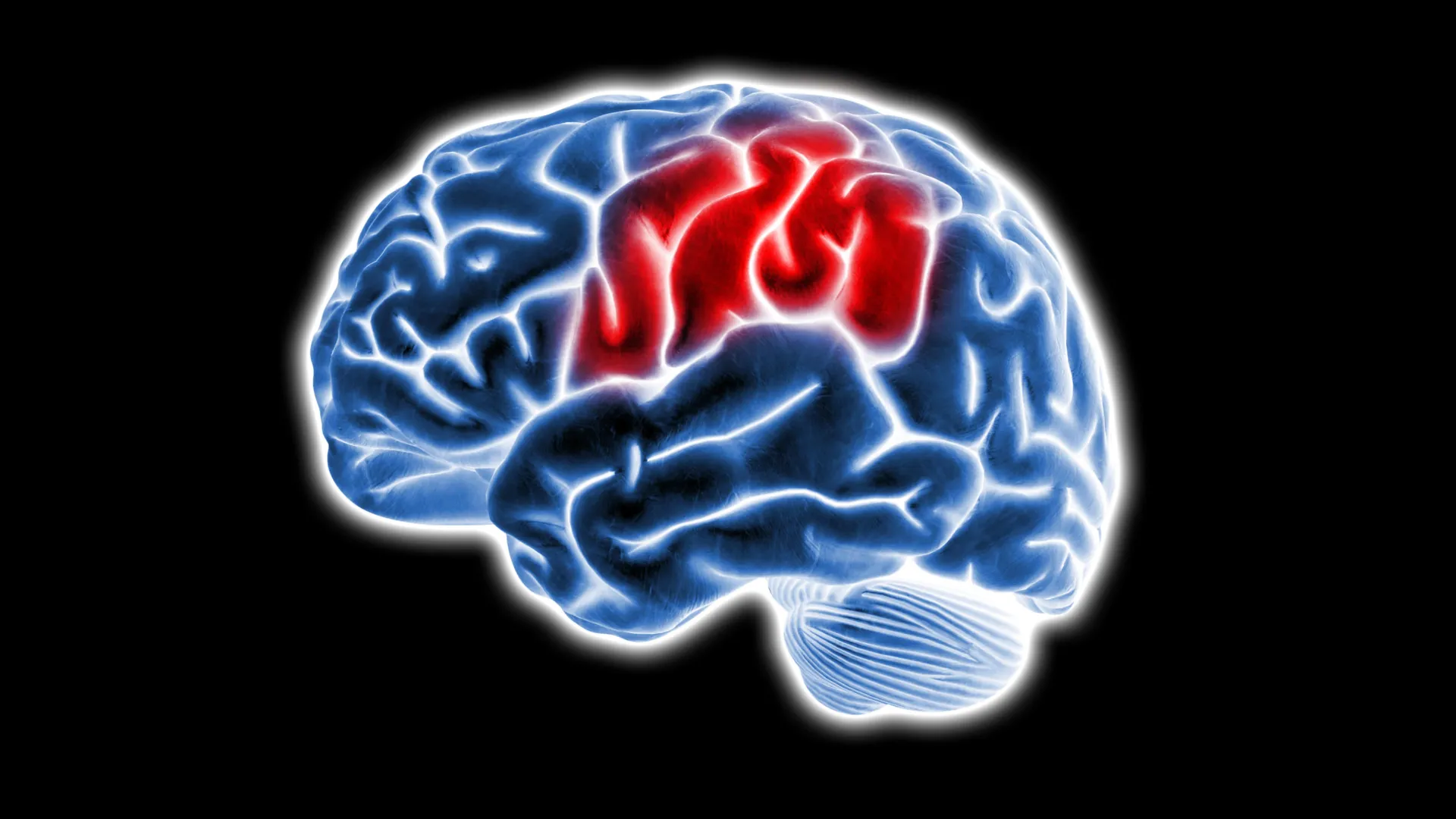
Scientists at Weill Cornell Medicine have identified a surprising culprit that may contribute to dementia: free radicals generated in a particular region of brain support cells known as astrocytes. The study, published Nov. 4 in Nature Metabolism, found that blocking this specific site reduced inflammation and protected neurons. The results point toward a promising new strategy for treating neurodegenerative diseases such as frontotemporal dementia and Alzheimer's disease.
"I'm really excited about the translational potential of this work," said Dr. Anna Orr, the Nan and Stephen Swid Associate Professor of Frontotemporal Dementia Research in the Feil Family Brain and Mind Research Institute and member of the Appel Alzheimer's Disease Research Institute at Weill Cornell, who co-led the study. "We can now target specific mechanisms and go after the exact sites that are relevant for disease."
How Mitochondria and Free Radicals Affect the Brain
The research focused on mitochondria, the cell's energy-producing structures that convert food into usable energy. In the process, mitochondria release reactive oxygen species (ROS) -- molecules commonly known as free radicals. At normal levels, ROS help regulate essential cell functions, but excessive or poorly timed production can damage cells.
"Decades of research implicate mitochondrial ROS in neurodegenerative diseases," said Dr. Adam Orr, an assistant professor of research in neuroscience in the Feil Family Brain and Mind Research Institute at Weill Cornell, who co-led the work.
Because of this connection, scientists have long tested antioxidants as a potential way to neutralize ROS and slow neurodegeneration. However, these clinical trials have largely failed. "That lack of success might be related to the inability of antioxidants to block ROS at their source and do so selectively without altering cell metabolism," Dr. Adam Orr explained.
A New Way to Stop Harmful Free Radicals
As a postdoctoral researcher, Dr. Orr developed a drug discovery platform designed to find molecules that specifically suppress ROS at individual mitochondrial sites while leaving normal functions intact. Through this approach, the team identified a group of compounds called S3QELs ("sequels"), which showed potential to block harmful ROS activity.
The researchers focused on Complex III, a mitochondrial site known for producing ROS that can leak into the rest of the cell, potentially causing damage. To their surprise, the excess ROS did not originate from neurons, but from astrocytes -- non-neuronal cells that provide structural and metabolic support to neurons.
"When we added S3QELs, we found significant neuronal protection but only in the presence of astrocytes," said Daniel Barnett, a graduate student in the Orr lab and the study's lead author. "This suggested that ROS coming from Complex III caused at least some of the neuronal pathology."
Further experiments showed that when astrocytes were exposed to disease-related factors such as inflammatory molecules or proteins linked to dementia (including amyloid-beta), their mitochondrial ROS production increased dramatically. Treatment with S3QELs suppressed much of this rise, while blocking other ROS sources did not have the same effect.
Barnett discovered that ROS oxidized certain immune and metabolic proteins involved in neurological disease, altering the activity of thousands of genes tied to inflammation and dementia.
"The precision of these mechanisms had not been previously appreciated, especially not in brain cells," said Dr. Anna Orr. "This suggests a very nuanced process in which specific triggers induce ROS from specific mitochondrial sites to affect specific targets."
Promising Results in Animal Models
When the team administered the S3QEL compound to mice engineered to model frontotemporal dementia, they observed reduced astrocyte activation, lower levels of inflammatory gene expression, and a decrease in a tau modification linked to dementia. Remarkably, these effects appeared even when treatment began after symptoms had already started.
Extended treatment improved lifespan, was well tolerated, and produced no significant side effects. Dr. Anna Orr attributes this to the compound's highly targeted action.
The team plans to continue developing the S3QEL compounds in collaboration with medicinal chemist Dr. Subhash Sinha, professor of research in neuroscience in the Brain and Mind Research Institute and member of the Appel Alzheimer's Disease Research Institute at Weill Cornell.
They also intend to investigate how disease-associated genes influence ROS production and whether certain genetic variants that raise or lower dementia risk might do so by altering mitochondrial ROS activity.
Changing How Scientists Think About Free Radicals
"The study has really changed our thinking about free radicals and opened up many new avenues of investigation," said Dr. Adam Orr. The potential of these findings to open new research approaches to inflammation and neurodegeneration is highlighted in the journal.
Story Source:
Materials provided by Weill Cornell Medicine. Note: Content may be edited for style and length.
Journal Reference:
- Daniel Barnett, Till S. Zimmer, Caroline Booraem, Fernando Palaguachi, Samantha M. Meadows, Haopeng Xiao, Man Ying Wong, Wenjie Luo, Li Gan, Edward T. Chouchani, Anna G. Orr, Adam L. Orr. Mitochondrial complex III-derived ROS amplify immunometabolic changes in astrocytes and promote dementia pathology. Nature Metabolism, 2025; DOI: 10.1038/s42255-025-01390-y
Cite This Page: