Blocking a single protein forces cancer cells to self-destruct
- Date:
- November 20, 2025
- Source:
- NYU Langone Health / NYU Grossman School of Medicine
- Summary:
- Researchers uncovered a powerful weakness in lung cancer by shutting down a protein that helps tumors survive stress. When this protein, FSP1, was blocked, lung tumors in mice shrank dramatically, with many cancer cells essentially triggering their own self-destruct mode. The work points to a fresh strategy for targeting stubborn lung cancers.
- Share:
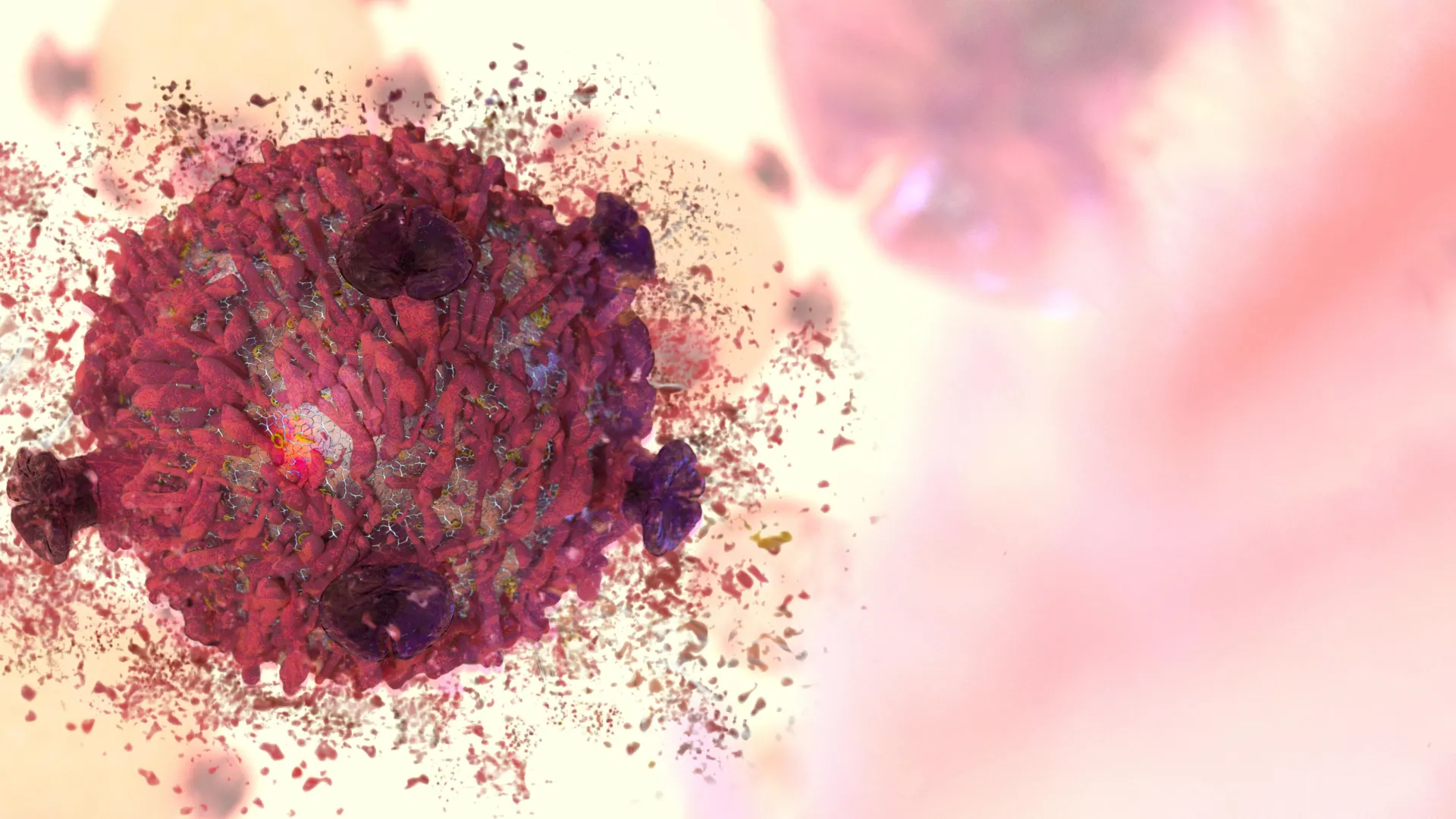
Researchers at NYU Langone Health have identified how a specific form of cell death linked to the buildup of highly reactive molecules can slow the growth of lung tumors.
This type of cell death, known as ferroptosis, originally evolved as a way for the body to clear out cells that become overly stressed. Cancer cells fall into this category, yet over time they have developed ways to block ferroptosis so they can continue multiplying even under damaging conditions.
Blocking FSP1 Dramatically Weakens Lung Tumors
A study published online November 5 in Nature showed that an experimental therapy targeting a protein called ferroptosis suppressor protein 1 (FSP1) significantly reduced tumor growth in mice with lung adenocarcinoma (LUAD). Blocking this protein, which helps cancer cells avoid ferroptosis, shrank tumors by as much as 80%. Lung cancer remains the world's leading cause of cancer-related deaths, and LUAD is the most common form among nonsmokers, accounting for about 40% of cases.
"This first test of a drug that blocks ferroptosis suppression highlights the importance of the process to cancer cell survivaland paves the way for a new treatment strategy," said senior study author Thales Papagiannakopoulos, PhD, an associate professor in the Department of Pathology at the NYU Grossman School of Medicine.
Reactive Molecules and Their Role in Cell Damage
Ferroptosis takes place when iron levels rise inside cells, fueling the production of highly reactive molecules made from oxygen, water, and hydrogen peroxide known as reactive oxygen species (ROS). In small amounts, ROS help cells communicate. In excess, they create oxidative stress, which occurs when ROS add oxygen molecules to vital proteins and DNA, damaging or breaking them apart. ROS can also harm fats that form the outer membranes of cells, contributing to cell death and tissue injury.
Blocking FSP1 Shows Strong Tumor-Suppressing Effects
To investigate how FSP1 affects lung cancer, the research team genetically modified mice so that their lung cancer cells lacked the FSP1 gene. These mice developed smaller tumors due to increased cancer cell death. The researchers also tested icFSP1, a newer drug designed to inhibit FSP1. Mice treated with icFSP1 lived longer and experienced tumor reductions similar to those seen in mice whose cancer cells were engineered to lack FSP1.
The study also found that FSP1 may be a more promising treatment target than another ferroptosis-blocking protein, glutathione peroxidase 4 (GPX4), which has been studied in cancer research for a longer period. The findings suggest that FSP1 is more actively involved in preventing ferroptosis in lung cancer cells while playing a smaller role in normal cell function (which could translate to fewer side effects). Increased levels of FSP1 were also associated with poorer survival rates in human LUAD patients, unlike GPX4.
Future Directions and Ongoing Research
"Our future research will focus on optimizing FSP1 inhibitors and investigating the potential of harnessing ferroptosis as a treatment strategy for other solid tumors, such as pancreatic cancer," said lead study author Katherine Wu, an MD/PhD student working in the Papagiannakopoulos lab. "We aim to translate these findings from the lab into novel clinical therapies for cancer patients."
In addition to Wu and Pagagiannakopoulos, contributors from the Department of Pathology at NYU Langone include co-first author Alec Vaughan, Jozef Bossowski, Yuan Hao, Aikaterini Ziogou, Mari Nakamura, Ray Pillai, Mariana Mancini, Sahith Rajalingam, and Suckwoo Chung. Other study authors include Seon Min Kim, Tae Ha Kim, and Yun Pyo Kang of the College of Pharmacy and Research Institute of Pharmaceutical Sciences at Seoul National University; Mingqi Han and David Shackelford from the Department of Pulmonary and Critical Care Medicine at the David Geffen School of Medicine, University of California Los Angeles; Toshitaka Nakamura and Marcus Conrad of the Institute of Metabolism and Cell Death, Molecular Targets and Therapeutics Center at Helmholtz Munich in Germany; and Lidong Wang and Diane Simeone of the Moores Cancer Center, University of California, San Diego, La Jolla.
The study received funding from National Institutes of Health grants S10RR027926, S10OD032292, R37CA222504, R01CA227649, R01CA283049, R01CA262562, T32GM136542, T32GM136573, and T32GM136542. Additional support was provided by the American Cancer Society Research Scholar Grant (RSG-17-20001-TBE), the Ruth L. Kirschstein Individual Predoctoral National Research Service Award fellowship (F30CA275258), the Deutsche Forschungsgemeinschaft (DFG) (CO 291/7-1 Priority Program SPP 2306 [CO 291/9-1, #461385412; CO 291/10-1, #461507177], the European Research Council under the European Union's Horizon 2020 research and innovation program (grant GA 884754), and the Perlmutter Cancer Center Support Grant P30CA016087.
Papagiannakopoulos received funding from the Pfizer Medical Education Group, Dracen Pharmaceuticals, Kymera Therapeutics, Bristol Myers Squibb, and Agios, available under a CC-BY-NC-ND 4.0 international license. These relationships are being managed in accordance with NYU Langone Health policies.
Story Source:
Materials provided by NYU Langone Health / NYU Grossman School of Medicine. Note: Content may be edited for style and length.
Journal Reference:
- Katherine Wu, Alec J. Vaughan, Jozef P. Bossowski, Yuan Hao, Aikaterini Ziogou, Seon Min Kim, Tae Ha Kim, Mari N. Nakamura, Ray Pillai, Mariana Mancini, Sahith Rajalingam, Mingqi Han, Toshitaka Nakamura, Lidong Wang, Suckwoo Chung, Diane Simeone, David Shackelford, Yun Pyo Kang, Marcus Conrad, Thales Papagiannakopoulos. Targeting FSP1 triggers ferroptosis in lung cancer. Nature, 2025; DOI: 10.1038/s41586-025-09710-8
Cite This Page: